- Dr. Nishad Matange’s work at IISER Pune aims to scientifically decipher how much antibiotic is enough or rather how much is too little. To do this, he and his students force bacteria into situations where only those with randomly emerging resistance genes survive. They then read out (sequence) what mutations the bacteria has acquired to fend off the antibiotic and their location in the genome.
- Prof. Dr. Paul Salins, Medical Director and Senior Vice President at the NH-Mazumdar Shaw Medical Centre, Bengaluru, points to the need for nature-based solutions to aid the efficacy of antibiotic treatment in case of infections and other medical challenges, including bacterial and other microbial invasions.
Antimicrobial resistance (AMR), aka the silent pandemic, refers to the increasing ability of microorganisms – largely bacteria but also other microbes – to resist currently available medical treatment. This may sound as though it is simply a relevant issue but here is why the problem needs immediate consideration:
The O’Neill Report—constituted by the UK National Health Service in 2014—projected the worst outcome for humanity and global health in the context of antimicrobial resistance (AMR). Unchecked, this phenomenon will lead to financial costs of up to US$100 billion and deaths in excess of 10 million associated with drug resistance by 2050.
The burden will, for the most part, fall on the Low and Middle-Income countries (LMICs), including India. The underlying driver of this predicted liability is the continuous evolution of bacterial defence mechanisms in the backdrop of ‘the great antibacterial innovation gap’. The term refers to the fact that the last time a new antibiotic class was discovered was in 1987 (the discovery of lipopeptides). To understand this relationship a little better, let us go back to an example that Sir Alexander Fleming gave during his Nobel lecture on 11th December 1945:
‘Here is a hypothetical illustration. Mr. X. has a sore throat. He buys some penicillin and gives himself, not enough to kill the streptococci but enough to educate them to resist penicillin. He then infects his wife. Mrs. X gets pneumonia and is treated with penicillin. As the streptococci are now resistant to penicillin, the treatment fails. Mrs. X dies. Who is primarily responsible for Mrs. X’s death? Why, Mr. X whose negligent use of penicillin changed the nature of the microbe. Moral: If you use penicillin, use enough.’
While this may sound like a very crude and simplified example, it is the reason we are facing a crisis now. Replace the word penicillin with ‘antibiotic’ and think of similar scenarios you might have experienced, read or heard of. We quickly realise that Dr Fleming, the discoverer of the first antibiotic in clinical use, illustrated the situation that renders more and more antibiotics less efficient if not useless, leaving us increasingly vulnerable to bacterial infections and resulting in the alarming numbers in the O’Neill report.
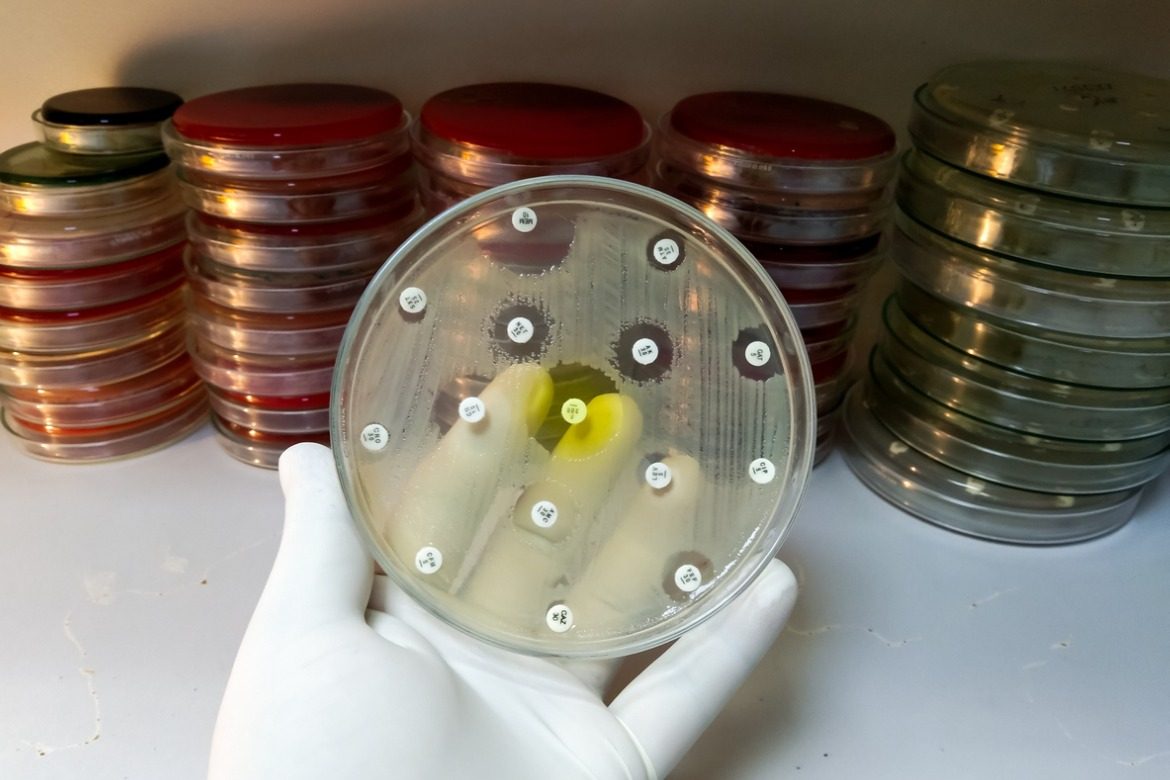
The scenario Dr Fleming described is the underlying inspiration for Dr. Nishad Matange’s work at IISER Pune. It aims to scientifically decipher how much antibiotic is enough or rather how much is too little. To do this, he and his students force bacteria into situations where only those with randomly emerging resistance genes survive. They then read out (sequence) what mutations the bacteria has acquired to fend off the antibiotic and their location in the genome. More importantly, they look at the prominent and other metabolic nodes of the bacterium that react to antibiotic stress.
This research is crucial as it can buy time in the battle against the spread of antibiotic resistance and the desperate search for new classes of antibiotics. It allows us to repurpose or reuse the existing pharmaceutical toolkit. While a bacteria may have been resistant to an antibiotic, it could be re-sensitised if a second compound is administered that compromises certain pathways of bacterial metabolism.
Let’s, for example, imagine a very demanding boss. Think of something else that also strains you, such as a very demanding client. While you may have been able to manage either of them separately, both of them in tandem could bring you close to a breakdown.
Dr. Matange’s group also aims to understand at what antibiotic concentration thresholds bacteria evolve resistance rather than die and how quickly bacteria tend to evolve resistant genes. Both questions are very relevant for researching and developing new classes of antibiotics, treatment protocols for clinicians, and good antibiotic stewardship. His group works not only with lab-grown strains but also with hospital strains – resistant bacteria recovered from patients. This is key to understanding and restraining such bacteria early.
Access to emerging resistant strains and their sequences is crucial if we want to stay on top of the situation. This is where Switzerland can benefit highly from research collaborations and open science. While India and Switzerland work closely together at higher levels, e.g. policy development and public health with players such as Global Antibiotic Research and Development Partnership (GARDP) and affordable diagnostics with organisations such as FIND, there is a lot of room for better collaboration. This is especially true when it comes to establishing and maintaining comprehensive databases that house information on emerging resistance genes and strains, including metadata such as prevalence, socio-economic and geographic context, exchange of knowledge and best practices in fundamental and clinical research and synergistic usage of skills and resources. We need a relationship built on trust, transparency, and a shared purpose to solve health problems that plague humanity.
Dr. Matange’s work is not the only beacon in the Indian AMR research community. The Bangalore-based biopharmaceutical start-up Bugworks has a novel small-molecule antibiotic, currently in phase 1 clinical trials in Australia. This broad-spectrum drug is expected to cover critical priority pathogens and biothreat pathogens resistant to last-line antibiotics such as carbapenems. Bugworks is incubated at the C-CAMP campus in Bangalore. C-CAMP’s international value can be seen in its selection as the only CARB-X accelerator outside of the Global North (EU and USA) and the trust the India AMR Innovation Hub partners placed in them late last year by joining a large multinational consortium to fuel cross-border AMR innovation.
Last but not least, Prof. Dr. Paul Salins, Medical Director and Senior Vice President at the NH-Mazumdar Shaw Medical Centre, Bengaluru, points to the need for nature-based solutions to aid the efficacy of antibiotic treatment in case of infections and other medical challenges, including bacterial and other microbial invasions. India has a long history of identifying and using plant-derived compounds. It will continue to use and further this knowledge to elevate the body’s defence mechanism, reducing the need for intervention with chemical-derived compounds to fight off infections. This is a potential partnership area to learn and grow together.
In summary, India is a relevant knowledge partner that can build cross-border health resilience through various paths.
(With inputs from Dr Nishad Matange, Dr Vasan K Sambandamurthy and Prof. Dr Paul Salins.)




NO COMMENT